Overview of Misophonia [TOP]
Misophonia is a recently identified disorder in humans which is characterized by an extreme emotional response of anger or disgust to commonly occurring, innocuous auditory or visual stimuli (Edelstein, Brang, Rouw, & Ramachandran, 2013; Jastreboff & Jastreboff, 2002, 2014; Schröder, Vulink, & Denys, 2013; Wu, Lewin, Murphy, & Storch, 2014). The condition was first identified in 1997 by audiologist Marsha Johnson, which she named Selective Sound Sensitivity Syndrome (4S; Bernstein, Angell, & Dehle, 2013). The name misophonia, which means “hatred of sound” was proposed by Jastreboff and Jastreboff (2002). The name misophonia refers to the emotions evoked by the trigger stimulus rather than a general hatred of sound.
Misophonia is a unique and discrete disorder that cannot be classified in the DSM-5 or IDC-10 (Schröder et al., 2013). With misophonia, specific auditory or visual stimuli trigger a response of irritation or disgust, which immediately escalates to anger (Schröder et al., 2013). Auditory triggers can be almost any repeating sound, but those commonly reported are eating sounds (e.g. lip smacking, chewing), nasal sounds (e.g. sniffing, breathing, snoring), and repetitive sounds (e.g. typing, pen clicking; Edelstein et al., 2013; Jastreboff & Jastreboff, 2014; Schröder et al., 2013; Wu et al., 2014). Visual trigger stimuli of repetitive movements (e.g. hair twirling, leg shaking) and movements associated with auditory triggers (e.g. jaw movement) are also reported (Jastreboff & Jastreboff, 2014; Wu et al., 2014).
Emotions commonly reported in response to trigger stimuli are anger and disgust (Edelstein et al., 2013; Johnson et al., 2013; Schröder et al., 2013; Wu et al., 2014). Schröder et al. (2013) noted that anxiety was specifically not a response to trigger stimuli of the participants in their study, but participants reported actively avoiding exposure to trigger stimuli. Other researchers have reported anxiety as a common emotion of individuals with misophonia (Edelstein et al., 2013; Johnson et al., 2013; Wu et al., 2014). Although this seems to be a discrepancy, the anxiety of misophonic individuals could have been associated with avoidance behaviors, and so referred to as avoidance by Schröder et al. (2013).
The physiologic response accompanying strong emotions was measured to validate self-reports of emotional responses to trigger stimuli (Edelstein et al., 2013). Skin conductance was shown to begin increasing 2 seconds after onset of trigger stimuli and continue increasing for the duration of a 15s trigger. Participants in this study also reported general physiologic responses associated with emotional arousal including pressure in chest, head, and whole body; clenched/tightened muscles; sweaty palms; difficulty breathing; and increased blood pressure and heart rate.
Although the prevalence of misophonia in the general population is unknown, it was estimated at 3.2% based on comorbidity with other auditory conditions (Jastreboff & Jastreboff, 2014). Another study utilizing undergraduate psychology students reported 20% of participants had clinically significant misophonia (Wu et al., 2014). Misophonia can develop at any age, with a mean age of onset in childhood (Schröder et al., 2013). Once misophonia develops, it seemingly persists over the lifespan of the individual and often worsens with time (Schröder et al., 2013). The impact on the individual can vary from mild to debilitating and can cause severe problems in family, social, and professional life (Dozier, 2015b; Edelstein et al., 2013). Although misophonia is a chronic condition, it can vary due to other factors. Patients have reported that the severity of their misophonia is affected by their momentary feeling of well-being (Wu et al., 2014).
Theoretical and Research Basis for Treatment [TOP]
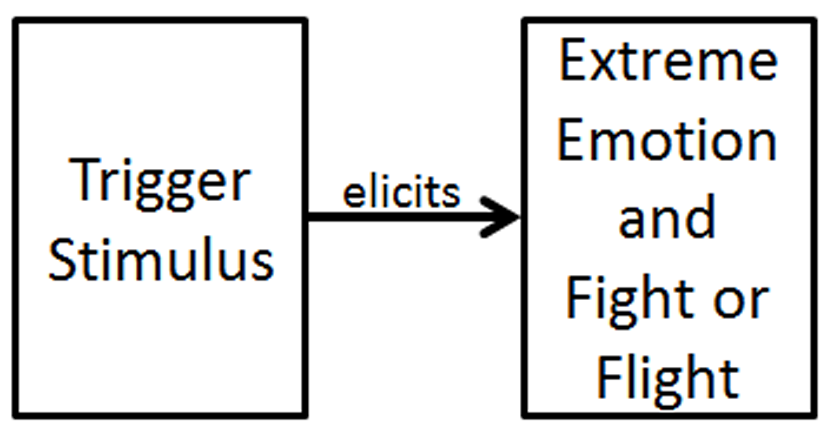
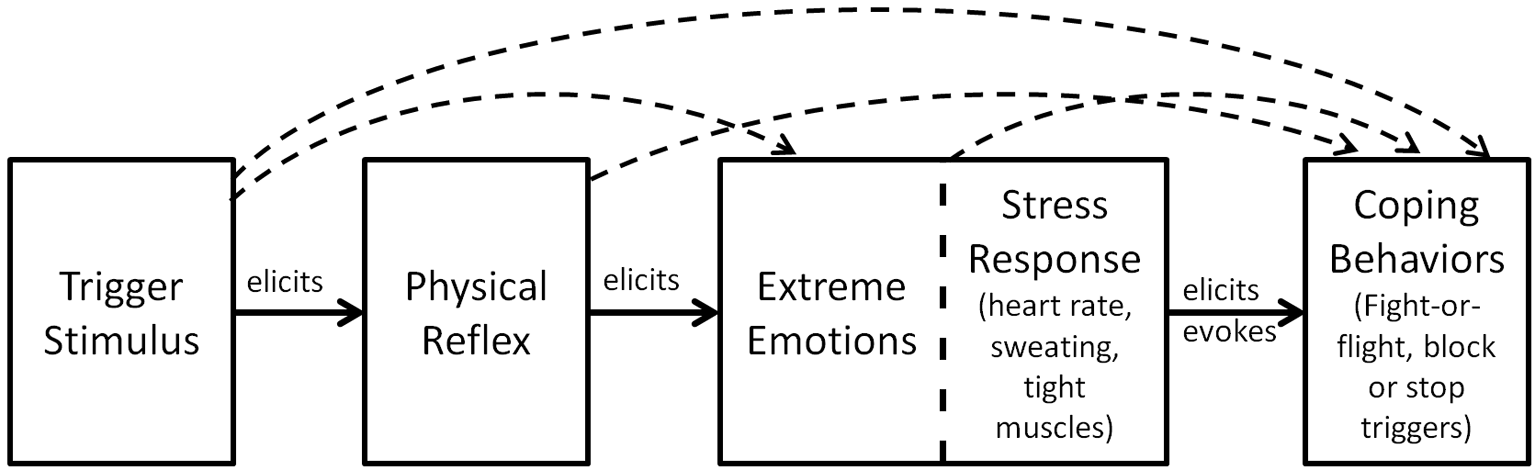
Research on the etiology and nature of misophonia is limited by the lack of an animal model (Jastreboff & Jastreboff, 2014). Studies to date have focused on the stimulus-emotion relationship and physiological responses accompanying strong emotions (Edelstein et al., 2013; Schröder et al., 2013; Wu et al., 2014). The etiology and nature of misophonia has been ascribed to physiological abnormalities in the brain (Møller, 2011), general hyper-reactivity similar to sensory processing disorder (Schröder et al., 2013), and classical conditioning (Dozier, 2015b; Jastreboff & Jastreboff, 2014; Schröder et al., 2013). Most discussions of misophonia refer to the condition as an emotional response to trigger stimuli, with accompanying fight-or-flight responses, including both physiological arousal and behavioral activation as shown in Figure 1 (Bernstein et al., 2013; Edelstein et al., 2013; Jastreboff & Jastreboff, 2002, 2014; Schröder et al., 2013; Wu et al., 2014).
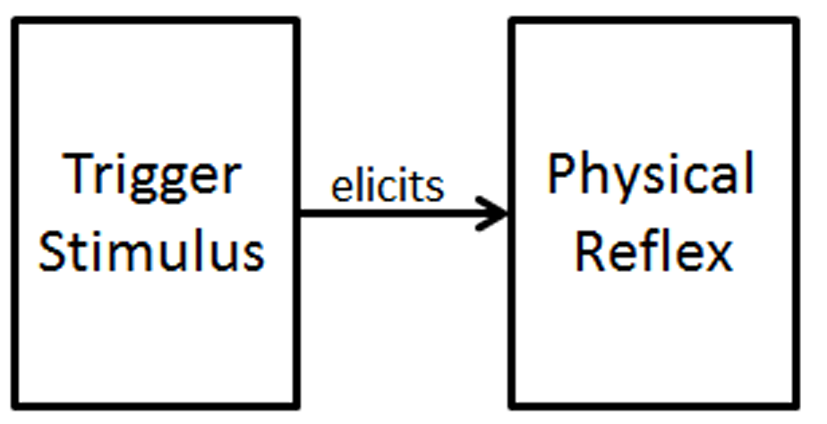
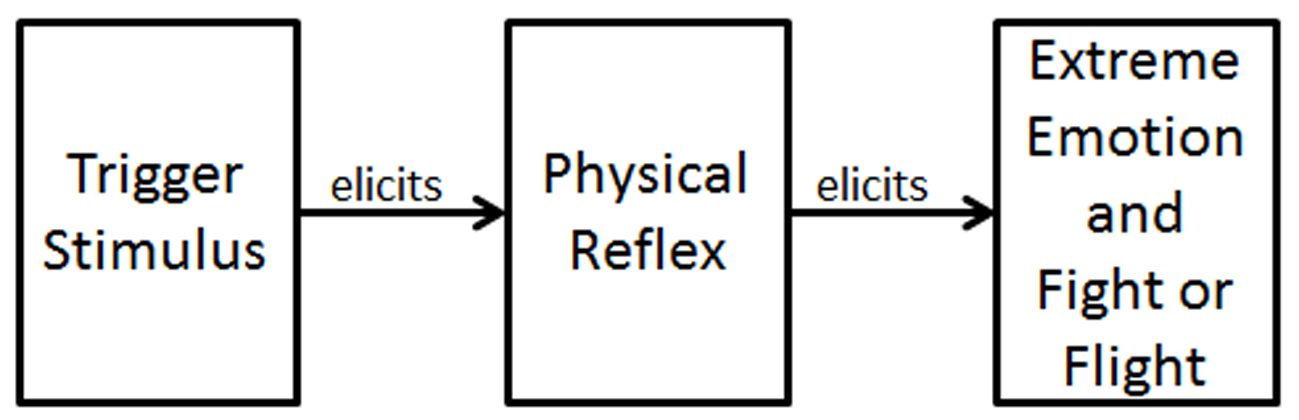
Dozier (2015a, 2015b) identified a discrete muscle reflex in response to trigger stimuli, which occurred independently of the emotional response when the trigger stimuli were sufficiently weak (see Figure 2). Dozier proposed that the emotional response may be elicited by the sensation from the physical reflex, because of the observed direct relationship between the decrease of the physical reflex in treatment and the decrease of the emotional response in real-life (see Figure 3).
Figure 2
Initial skeletal reflex response to a misophonic trigger stimulus. The trigger stimulus directly elicits a skeletal muscle contraction.
As shown in Figures 1, 2, and 3, the trigger stimulus elicits a response. Such a stimulus-response pair is known as a reflex. A Pavlovian conditioned reflex is generally viewed as being learned through a temporal pairing of a neutral stimulus (NS), which becomes the conditioned stimulus (CS), and an unconditioned stimulus (US), such that the CS becomes associated with the US and elicits a response similar to the unconditioned response (UR) elicited by the US (Lattal, 2012). It has been demonstrated that the critical pairing for conditioning to occur is the NS/CS with the UR (Donahoe & Vegas, 2004), rather than that of the NS/CS and the US. When a stimulus occurs 0 to 2 seconds prior to a skeletal reflex response, Pavlovian conditioning can occur (Furedy & Riley, 1987, p. 7), and that stimulus can then elicit a conditioned response.
Treatment of Misophonia [TOP]
There have been no controlled studies on the treatment of misophonia, but there are several published case studies and summaries of patient outcomes. The most established method of treating misophonia is to add noise to the patient’s environment, which reduces the misophonic response to auditory triggers (Jastreboff & Jastreboff, 2014; Johnson, 2014). This is generally accomplished with a behind-the-ear sound generator that resembles a small hearing aid. Additionally, this treatment has incorporated protocols to promote active extinction of the misophonic response (Jastreboff & Jastreboff, 2014) or cognitive behavioral therapy to manage misophonia as a chronic condition (Johnson, 2014). Both methods have reported a high level of positive patient outcomes, but details on attrition, statistical significance, and effect size have not been reported.
A case study of cognitive behavioral therapy (CBT) to treat misophonia in a young woman reported remediation of impaired social functioning at end of treatment and at 4-months posttreatment, although the woman still found the trigger stimuli unpleasant (Bernstein et al., 2013). Another CBT case study reported successful reduction in maladaptive behavior associated with trigger stimuli in two adolescents (McGuire, Wu, & Storch, 2015), but no follow-up data was provided. A third case study reported using a counterconditioning treatment called the Neural Repatterning Technique (NRT) in a middle-aged woman by individually counterconditioning three auditory triggers and a visual trigger (Dozier, 2015a). This treatment paired a continuous positive stimulus with an intermittent, reduced-intensity trigger stimulus which resulted in a progressive decline in the strength of her physical reflex to the trigger stimulus (see Figure 2). The patient reported a decline in her emotional responses to real-life trigger stimuli which accompanied the decline in her physical reflex during treatment (see Figure 3). The patient reported a large reduction in the severity of her misophonia at the end of treatment, and at 4- and 10-months posttreatment.
At the 2013 Misophonia Association Conference, a member of the patient panel reported virtually eliminating his misophonic emotional response by relaxing all of his muscles continually during a trigger situation (Martz, 2013). Discussion with the author revealed that this individual developed proficiency in progressive muscle relaxation (PMR) as a treatment for his general anxiety as a teenager, and for many years he relaxed his muscles immediately after triggers to suppress his emotional response.
Progressive Muscle Relaxation [TOP]
Progressive Muscle Relaxation (PMR) is practiced by systematically tensing and relaxing 15 to 20 skeletal muscle groups (Borkovec & Sides, 1979). It has been demonstrated that individuals who practice PMR develop increased control of skeletal muscles, including a reduction in muscle tension during stressful events (Borkovec & Sides, 1979; Lehrer, Woolfolk, Rooney, McCann, & Carrington, 1983; O'Bannon, Richard, & Runcie, 1987). Daily PMR has been shown to be a benefit in treating anxiety disorders and improving well-being (Borkovec & Sides, 1979; Conrad & Roth, 2007; Dehghan-Nayeri & Adib-Hajbaghery, 2011; O'Bannon, Richard, & Runcie, 1987; Öst, 1987, 1988a).
Applied Relaxation is an enhancement to PMR that incorporates PMR as the initial relaxation training (Conrad & Roth, 2007; Öst, 1987, 1988b). The second phase of training includes relaxing each muscle group sequentially without first tensing it. The final phase develops the skill of relaxing all muscles simultaneously. Applied relaxation is the technique which was ascribed as an effective management technique for misophonia by one misophonic individual (Martz, 2013).
Application to Case [TOP]
There is little absolute certainty about misophonia due to the sparse research on the condition, except the finding that typically innocuous auditory and visual stimuli evoke extreme, involuntary emotional responses in the misophonic individual (see Figure 1). Misophonia is a chronic condition that generally maintains or strengthens, so it is unlikely that the condition will abate without intervention. Of fundamental interest to this case is the view of misophonia as a conditioned reflex response and therefore subject to change through experience, as reported by two misophonia treatment providers (Dozier, 2015a; Jastreboff & Jastreboff, 2014). The physical reflex response of misophonia, as shown in Figures 2 and 3, identifies a characteristic that is germane to this case. The course of treatment was informed by the research on muscle relaxation which indicates that the daily practice of PMR provides broad wellness benefits in addition to developing improved muscle control.
Case Description [TOP]
Presentation [TOP]
Miley (pseudonym) was a 21-year-old, single Caucasian woman. She attended university during the school year, but had just moved home for the summer. Her mother was divorced and lived alone. Miley reported having a generally positive relationship with her mother, except for the issue of misophonic triggers by her mother, which made living together difficult. Miley was not taking psychotropic medications. She presented for treatment by VSee video-chat and was well-groomed, articulate, and outgoing, with an overall positive attitude toward life which was reflected in her bright smile and cheerful demeanor. (VSee is a medical-grade internet video chat service that meets the confidentiality requirements for treatment of patients).
Presenting Complaints [TOP]
Miley contacted the author by email seeking treatment for misophonia after she had self-diagnosed her condition based on internet research. She was far from the treatment facility, so assessment and treatment were provided by VSee. Although her misophonia caused extreme emotions and was a major problem for her at university, she requested help with the misophonic triggers from her mother, which specifically were sounds of chewing and scraping of utensils on dishes. She reported extreme emotions of anger and rage in response to being triggered by her mother, which prevented them from eating together.
History [TOP]
Miley reported that her misophonia began at about age 6 or 7, but her first concrete instance of a severe response to a trigger was at age 9. Her first triggers were her mother’s yawning and gum chewing, and a classmate yawning. She reported that her childhood seemed fairly normal to her. She viewed herself as overweight at age 6 and tried to diet at age 8. Her parents divorced when she was 8, but she didn’t feel overly affected by this or other life events. She reported that she was a sensitive child, who responded to her mother’s emotions and that her mother was often stressed. Miley reported that she had never been diagnosed with depression, anxiety, or other mental conditions, and that she did not have any such tendencies.
Assessment [TOP]
All assessment forms were downloaded from misophoniatreatment.com and submitted by email, including an informed consent. The questionnaires included the Misophonia Assessment Questionnaire (MAQ) and the Misophonia Coping Responses (MCR) surveys by audiologist Marsha Johnson, which she has used in her practice for over a decade. The MAQ contains 21 questions on time spent with various negative thoughts and feelings about misophonia. The rating scale is 0 to 3, with 3 being “almost all the time” and 0 being “none of the time” so the sum score can range from 0 to 63. Johnson (2014) used the sum MAQ score to rate patient misophonia severity as mild (1-21), moderate (22-42), or severe (43-63). Other questionnaires included the Misophonia Activation Scale (MAS-1) from misophonia-UK.org, Misophonia Physical Sensation scale (MPS) and Misophonia Trigger Severity scale (MTS) by audiologist Natan Bauman, and the Misophonia Emotional Response (MER) survey by the author. See Appendices 1-6 for the specific content of the assessments and patient responses. Presently there are no validated misophonia assessment instruments.
The written assessment was based solely on the self-report of the client. Her responses supported her self-diagnosis of misophonia. Miley’s responses on the MAQ showed that she had a high level of preoccupation with misophonia, answering 16 of the 21 questions with “a good deal” or “almost all of the time,” and the other 5 with “a little of the time.” Her sum score was 49 at intake, which rated her misophonia as “severe.” Miley’s initial rating for her emotional distress to triggers was 9 on the MAS-1, and her physical sensation was 7 on the MPS. Her rating was 8 on the MTS, which is a combination of emotional and physical response severity (see Table 1).
Table 1
Assessment Measures
| Assessment instrument | Time of measurement
|
|||
|---|---|---|---|---|
| Intake | End of treatment | 6-month follow-up | 12-month follow-up | |
| Misophonia Assessment Questionnaire (MAQ)a | 49 | 13 | 7 | 12 |
| Misophonia Activation Scale (MAS-1)b | 9 | 4-7 | 4d | 10e |
| Misophonia Physiological Scale (MPS)b | 7 | 2 | 2f | 2f |
| Misophonia Trigger Severity (MTS): Spoon-on-bowlb | 8 | 1-2 | 0 | 0 |
| Misophonia Trigger Severity (MTS): Chewingb | 8 | 2 | 0-2 | 0 |
| Misophonia Trigger Severity (MTS): Other triggersc | 8 | 8, 11, 12 | 0-3, 11 | 0, 1, 8, 11, 12 |
aValues are sum scores. bValues are maxima. cMultiple ratings indicate response variability. dMode = 1. eMode = 3. fMode = 0.
On the MCR survey Miley reported that she usually responded to triggers with mild responses that indicated she was annoyed or upset, or by turning away or covering her eyes, putting on headphones, moving away from the sound, and leaving the room either immediately or after attempting to tolerate the sound. She reported often engaging in more aggressive responses, in that she would sternly ask the triggering individual to stop making the sound, verbally snap at the person making the sound, or use physical violence on the person making the sound. Her individual responses are shown in Appendix 2.
Miley’s emotional responses to triggers were extreme. All of her responses on the MCR were “almost all the time” except for nonaggressive feelings such as wishing she were deaf, not wanting to offend, or feeling hopeless. She also rated herself low on feeling offended by the person making the sound and feeling disgust. Her individual responses are shown in Appendix 6.
Miley’s responses on the assessments indicated that she was suffering from misophonia. To confirm this diagnosis, the therapist tested for an immediate physical reflex response to a single instance of a trigger stimulus (see Figure 2 and Figure 3). The therapist asked Miley to close her eyes and relax while he used a spoon and a bowl to make a trigger sound. The therapist’s first trigger sounds were intentionally too soft and short to trigger the patient. The therapist then increased the volume and duration of the sound until Miley reported that she was triggered. She reported that she felt the response in her hands and forearms as if to make a fist, which indicated that the muscle that contracted was probably the flexor digitorum profundus in her forearms.
Treatment [TOP]
Treatment Conceptualization [TOP]
Misophonia is characterized as an involuntary response to a trigger stimulus. A counterconditioning treatment (i.e., NRT treatment) was reported as being effective in the treatment of specific trigger stimuli for a middle-aged woman (Dozier, 2015a) whose misophonic responses consisted of a physical reflex response to the trigger stimuli and an emotional response. It was posited that the physical reflex response mediated the emotional response, as shown in Figure 3 (Dozier, 2015b). The NRT treatment described by Dozier (2015a) focused on eliminating the physical reflex response without addressing the emotional response. In that case, reducing or eliminating the physical response reduced or eliminated the emotional response in real-life settings. The counterconditioning treatment was delivered in a weekly session with the therapist and with custom audio recordings for daily, independent sessions by the patient. A treatment app (Misophonia Trigger Tamer) was developed by the author for smartphones to automate the delivery of the NRT treatment. The app delivered a continuous positive auditory stimulus (music) and intermittently delivered the trigger stimulus. The app provided control for volume, duration, and rate of the trigger stimulus, which allowed the patient real-time control of the treatment. The app also had the capability for the patient to record and edit custom trigger stimuli, and use their choice of music for the positive stimulus. Delivery of the positive stimulus with the app is optional. The positive stimulus could also be provided by another activity such as a taking a walk or viewing photographs.
Misophonia is reported to persist and often worsen with time (Schröder et al., 2013). Therefore, if misophonia includes a conditioned physical reflex response to the trigger, there must be a mechanism that allows Pavlovian conditioning to occur, such that the trigger-response reflex is maintained or strengthened. Dozier (2015b) posited that the pairing of the trigger stimulus and an increased intensity response can occur when the individual receives repeated triggers. Firstly, muscle tension may increase if the muscle affected by the trigger is not relaxed before the subsequent trigger stimulus, especially when the trigger stimuli occur at high rate. Secondly, a heightened state of anger and distress is experienced with misophonic triggers, and this generally increases muscle tension, which could also contribute to the maintenance of the conditioned reflex. To achieve the opposite effect, an individual would need to relax the affected muscle and remain calm while experiencing repeated trigger stimuli.
As previously discussed, Progressive Muscle Relaxation (PMR) has been demonstrated to increase deliberate control of relaxing a specific muscle; therefore, engaging in PMR for sufficient time to develop muscle control prior to the counterconditioning treatment may enhance the treatment effect. Relaxing muscles in response to triggers, as is taught in Applied Relaxation, might also reduce the emotional upheaval of a trigger situation, as previously discussed (Martz, 2013). Because of the broad benefits of daily deep relaxation, including reduction in anxiety, the author viewed PMR as a practice with the potential to enhance the therapeutic effect of treatment either directly or indirectly.
The treatment design for this case was essentially an automated version of the NRT treatment presented in Dozier (2015a) with the addition of Progressive Muscle Relaxation to develop muscle control and Applied Relaxation during treatment and when exposed to real-life trigger stimuli.
Course of Treatment [TOP]
The initial session included the assessment and a discussion on misophonia including ways to manage the condition. The topics covered were 1) the reflexive nature of misophonia; 2) how to reduce triggers by adding noise to the environment; 3) the importance of not enduring triggers; 4) an explanation of the NRT treatment; 5) selecting a the first trigger to address in treatment; 6) selecting the positive stimulus for treatment; 7) verification that Miley had the capability to set up her smartphone for treatment; and 8) a discussion of Progressive Muscle Relaxation. Miley was instructed to download the Misophonia Trigger Tamer app from iTunes or Google Play, learn to use it with the tutorial videos, set up the playlist and trigger in the app, and practice PMR twice a day.
Miley committed to performing the PMR exercise twice a day for the next week using online training video and guided audio downloads. She also committed to conducting four to six NRT 30-minute treatment sessions per week. All NRT treatments were to be carried out independently using the Misophonia Trigger Tamer app. All sessions with the therapist were to be conducted by VSee, which is a Health Insurance Portability and Accountability Act (HIPAA) compliant video-chat service.
Miley performed PMR twice each day for the 7 days before the second therapist session. At this session, she reported that relaxing her hands had reduced her emotional response when she was triggered in public, but that adding noise to her environment had not been effective in reducing her misophonic physical and emotional responses at home. During the previous week she recorded a spoon-on-bowl trigger and edited it, so that the trigger sound began immediately at the start of the file. She also set up a playlist in the Misophonia Trigger Tamer with a mixture of calming and happy songs to use as the positive counterconditioning stimulus. The session with the therapist included discussion about how to set the app parameters for the NRT treatment and a 5-minute sample NRT treatment to insure Miley knew how to conduct the treatment and that the parameters were properly set. She was instructed to increase the volume and duration of the trigger to maintain a low physical response of approximately 1 on a 0 to 5 scale, where 0 was no reflex response and 5 was a real-world trigger response. Miley was instructed to complete the 30-minute NRT treatment session she started with the therapist, and to perform a 30-minute treatment each day. The therapist recommended that she keep her hands relaxed during treatment sessions and wiggle her fingers when triggered in real life.
At the third session with the therapist, Miley reported that she had performed PMR every day and the NRT treatment on 3 days. She stopped after the third treatment because she no longer triggered to the recorded stimulus. She was instructed to use 2 other trigger recordings of the spoon-on-bowl sound and start a variety of chewing-sound triggers once she did not respond to the spoon-on-bowl triggers. She was instructed to continue daily PMR, relax her hands when triggered in real life, and continue with daily NRT treatments.
At the fourth therapist session, which was 2 weeks later, Miley reported that she had performed PMR most days. She happily announced that her responses to the spoon-on-bowl and chewing triggers were gone for her recorded sounds, but still small in real life. At this point, Miley chose to terminate treatment. She had conducted the 5, 30-minute NRT treatment sessions and 4 shorter sessions. The total time was equivalent to 7 half-hour NRT sessions. The Misophonia Trigger Tamer app history log is shown in Table 2. There are 9 entries, indicating that Miley heard a total of 368 spoon-on-bowl triggers and 178 chewing triggers. The duration of the triggers was 0.9s for the spoon-on-bowl triggers and 1.3s for chewing triggers. The inter-stimulus interval was 21 seconds.
Table 2
Misophonia Trigger Tamer History: This is the record of the treatments logged in the Misophonia Trigger Tamer app
| Start Date/Time | Planned Treatment Duration | Time of Last Trigger Played | Playlist Name | Trigger Name | Number of Triggers | |
|---|---|---|---|---|---|---|
| 1 | 5/29/2014 15:46 | 30:00 | 29:27 | Lizard Brain | Porcelain | 78 |
| 2 | 5/30/2014 14:05 | 30:00 | 29:25 | Lizard Brain | Porcelain | 78 |
| 3 | 5/31/2014 20:58 | 30:00 | 29:27 | Lizard Brain | Porcelain | 78 |
| 4 | 6/10/2014 09:44 | 30:00 | 29:24 | Lizard Brain | Porcelain 3 | 78 |
| 5 | 6/11/2014 16:44 | 30:00 | 22:13a | Lizard Brain | Porcelain 3 | 56 |
| 6 | 6/11/2014 17:14 | 30:00 | 09:52a | Lizard Brain | Chewing 1 | 24 |
| 7 | 6/15/2014 12:48 | 30:00 | 29:33 | Lizard Brain | Chewing 3 | 75 |
| 8 | 6/17/2014 10:23 | 30:00 | 23:00a | Lizard Brain | Chewing 3 | 58 |
| 9 | 6/18/2014 12:04 | 30:00 | 08:35a | Lizard Brain | Chewing 3 | 21 |
aTreatment terminated early.
Assessment of Progress [TOP]
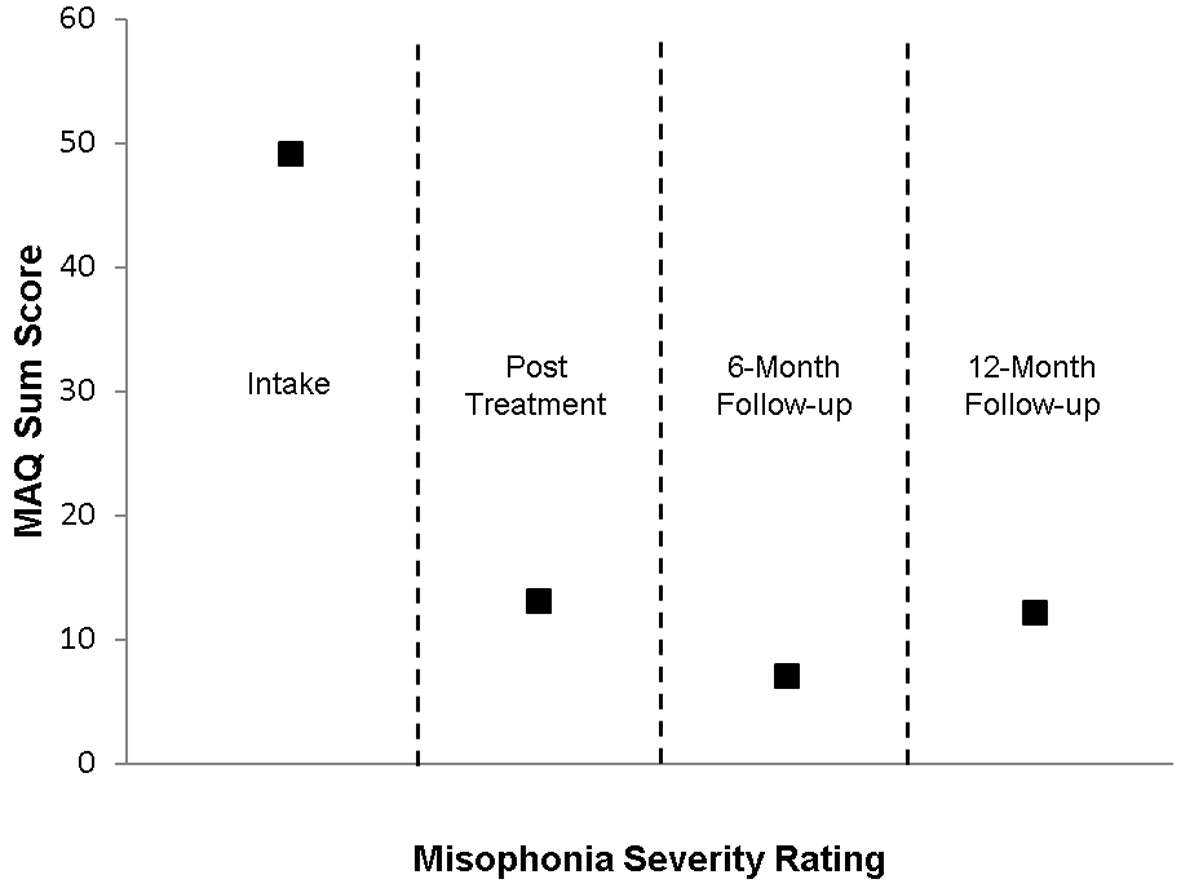
A summary of all assessment scores are shown in Table 1. Miley completed the MAQ, the MAS-1, and the MPS for her misophonia in general. Her MAQ sum score had declined from 49 to 13, indicating a sharp reduction in her general level of distress due to misophonia. Individual MAQ responses are shown in Appendix 1. Miley gave a range of 4 to 7 on the MAS-1 and a rating of 2 on the MPS. She completed the MTS for the specific triggers treated, and another MTS for triggers that had not been treated. Her MTS rating for the spoon-on-bowl trigger had declined from an 8 (“I feel physical sensation which can be best described as emotional pain and causes very strong emotions”) to 1-2 (“I feel some sensation and can ignore it” or “I feel some physical sensation but can often/always ignore it.”) Her MTS rating for chewing triggers had declined from 8 to 2. Her MTS ratings for non-treated triggers were 8, 11, and 12. Ratings of 11 and 12 are “no physical sensation” but “immediately feel anger or rage.”
Follow-Up [TOP]
The therapist followed up with Miley by email a month after she returned to university. She reported that her misophonia was still a significant problem, especially for yawning, which was both a visual and auditory trigger. She wrote that her response to yawning the previous semester was a 9 or 10, but this semester the worst she had experienced was a 5 and it was usually about a 3. (This verbal report did not reference any specific misophonia assessment scale).
Miley completed the assessment forms and returned them by email for a 6-month posttreatment assessment (see Table 1). Her MAQ sum score had declined to 7, and three of those points were her response to the item, “My sound issues do not seem to have a known cause.” (See Appendix 1 for specific responses). The large reduction in her MAQ sum score is illustrated in Figure 4. Her responses on the MCR survey indicated that she had a greatly reduced overt behavioral response to triggers. Her predominant responses to triggers were to “hear a known trigger sound . . . and feel no physical sensation” and “calmly move away from the sound.” (See Appendix 2). She also reported greatly reduced emotional responses to triggers. On the intake MER survey, 20 of the 26 responses were “almost all the time.” At 6-month follow-up, her highest response was “a good deal of the time” for feeling that she must see the person making the sound. Fourteen responses were “not at all” and 11 responses were “a little of the time.” (See Appendix 6). This large decline in the emotional distress to triggers was consistent with the decline in her MAQ sum score. Her MAS-1 score was 4, with a note that 1 was the typical response. Her MPS score was 2, with 0 being a typical response. The MTS score for spoon-on-bowl triggers was 0, and the response for chewing triggers was 0-2. The MTS scores for non-treated triggers was 0 to 3 and 11.
A second follow-up was conducted by email at 12 months posttreatment (see Table 1, Figure 4, and Appendix 1). Miley’s misophonia severity had increased as evidenced by the increase in the MAQ sum score to 12 and MAS-1 typical response rating to 3. She also indicated an increase the severity of her response to triggers that had not been addressed in treatment (MTS scores of 0, 1, 8, 11, and 12, indicating that she occasionally experienced rage in response to triggers). However, the triggers specifically addressed in treatment had completely extinguished (MTS score of 0). She also reported that she had been recently diagnosed with generalized anxiety disorder.
Complicating Factors, Access, and Barriers to Care [TOP]
There were no complicating factors such as difficulty creating appropriate materials for homework sessions as previously reported by Dozier (2015a). The Misophonia Trigger Tamer app allowed Miley to personally adjust the treatment parameters in response to changes in her physical response to the recorded trigger stimulus, so treatment was maintained at the prescribed level. The app also allowed Miley to record real instances of her triggers, edit them, and use them for treatment. The treatment did place a sizeable time demand on Miley. She was very diligent in performing the PMR exercises during the first week, but was sporadic with the NRT treatments, conducting these treatments on only 8 of the 21 days from start to end of treatment. The lack of compliance to the number of NRT treatment session was irrelevant due to her high rate of progress with the treatment. There were few, if any, issues with access or barriers to care in this case. The automation with Misophonia Trigger Tamer app reduced the therapist time to less than half of that required to provide the treatment manually, thereby greatly reducing the cost of treatment. VSee video-chat allowed the treatment to be provided over a long distance, and there were no interruptions to service.
Discussion [TOP]
Treatment Implications of the Case [TOP]
This case includes a replication plus an extension of the treatment of misophonia reported in Dozier (2015a). The replicated issues of treating misophonia include the following: 1) the NRT treatment effectively ameliorated the misophonia in the patient; 2) there was a physical reflex response to the trigger stimulus as shown in Figure 2; 3) the physical reflex occurred independently of the emotional response during treatment; 4) the physical reflex acted like a Pavlovian conditioned reflex in the gradual decline to exposure; and 5) there was a direct relationship between the reduction of the physical reflex and the reduction of the emotional response in real-world experience after treatment, supporting the relationship between the physical reflex and the emotional response shown in Figure 3. This case extended the treatment of Dozier (2015a) by incorporating the Misophonia Trigger Tamer app as an automated delivery mechanism for the NRT treatment, PMR, and Applied Relaxation in the NRT sessions.
Further support that misophonia is a conditioned response comes from the observation of spontaneous recovery by the patient. Spontaneous recovery of conditioned reflexes is a well-documented phenomenon, wherein the reflex decays during an active extinction process and then recovers with time (Lattal, 2012). The Misophonia Trigger Tamer app has precise settings for the volume and duration of the trigger stimulus in treatment. When the parameter values at the end of a treatment were used at the beginning of the next treatment, the response to the trigger was initially stronger than at the end of the previous treatment. This is consistent with spontaneous recovery of a conditioned reflex. Identifying misophonia as a conditioned reflex phenomenon has important implications for management, treatment, and research.
Firstly, with Pavlovian conditioning, a neutral stimulus that occurs temporally with a conditioned stimulus can become a conditioned stimulus. For misophonia, this means that a nontrigger stimulus (e.g., jaw movement) occurring with a trigger stimulus (e.g., chewing sound) can become a new trigger. As noted in Dozier (2015a), a visual trigger will continue to be a trigger, even after the response to the associated auditory stimulus has been extinguished. The implication here is that individuals should be cautious about repeated exposure to trigger stimuli because of the possibility of acquiring new triggers. This is an issue for managing misophonia as a chronic condition and exposure to triggers during treatment. Any treatment that includes exposure to triggers should include techniques that effectively reduce the misophonic response or are devoid of consistent pairing of nontrigger stimuli with trigger stimuli.
Secondly, viewing misophonia as a conditioned reflex rather than the result of a neurological defect has broad treatment implications. There is a large body of research on Pavlovian conditioning that may be applicable to the development and enhancement of treatment procedures (Donahoe & Vegas, 2004; Furedy & Riley, 1987; Lattal, 2012; Mowrer & Klein, 2000; Pavlov, 2003/1927). One simple application is that treatment should include techniques that will reduce a fundamental misophonic reflex rather than solely attempting to reduce the overt coping response of the individual. Jastreboff and Jastreboff (2014) reported achieving meaningful reduction of misophonia severity in patients with a treatment protocol that included in vivo counterconditioning experiences, along with other management techniques.
Thirdly, there is an implication for research to understand misophonia. It has been proposed that misophonia is the result of a defective or malfunctioning structure in the upper brain (Møller, 2011), which is diametrically opposed to the view that misophonia is a Pavlovian conditioning phenomenon. Viewing misophonia as anomalous brain activity will bias the researchers toward looking for the cause of misophonia within the brain, compared to viewing misophonia as an aversive conditioned reflex which is a result of typical brain functioning and environmental experience.
Limitations [TOP]
A case study has inherent limitations of generalizability and demonstration of causal factors. A controlled study is needed to demonstrate a causal relationship between the intervention and the reduction of misophonic symptoms. The patient’s initial physical misophonic reflex was a hand grasp, which seems easier to willfully control, and so may have facilitated response to treatment. Many individuals have a physical reflex that is more difficult to relax than a hand grasp. Additionally, the dependent measures were self-reports of the patient which is a limitation to the reliability of the data. The subject in this case demonstrated a high level of self-efficacy and motivation by seeking treatment, which could have been a factor for her rapid response to treatment. Furthermore, there was no formal assessment of comorbid conditions which could have an effect on the case.
Physical Misophonic Reflex and Progressive Muscle Relaxation [TOP]
The forearm muscle contraction Miley experienced in response to triggers appeared to be an important factor in the manifestation of her misophonia. Identifying the specific physical reflex response in the assessment allowed her to increase the focus on that specific muscle in her PMR exercises. Relaxing a hand grasp is a common behavior, so it is likely that Miley’s ability to relax this muscle during treatment was not based solely on one week of PMR exercises. Control of the affected muscle seems to have contributed to an enhanced effect of the NRT treatment because she could willfully relax those muscles during treatment and when triggered in real life. Individuals with other muscle reflexes may require much more practice to gain control of the muscle affected by a misophonia trigger and hence receive the benefit of relaxing during NRT treatments.
In both this case and that which was discussed in Dozier (2015a), the NRT treatment was effective in reducing specific triggers, but the reduction of treated triggers did not reduce non-treated triggers. By relaxing her hands in treatment, Miley developed a method of responding to real-life trigger situations that reduced her future misophonic response. This is supported by the decline in her response to triggers from her posttreatment assessment to the start of semester email report, and then the 6-month follow-up assessment at the end of the semester. In this case, Miley developed the ability to relax the affected muscles, and relaxing those muscles in trigger situations was a likely cause for the gradual reduction of her misophonic response for non-treated triggers. However at the 12-month follow-up assessment, she reported an increase in her emotional response to triggers, but she reported that her physical reflex response had remained low. Her increased emotional response to triggers may have been related to her recent diagnosis of generalized anxiety disorder.
Self-Treatment of Misophonia [TOP]
This case demonstrated the successful use of the Misophonia Trigger Tamer app to deliver the NRT treatment. All NRT treatment sessions were conducted independently by the patient. Because the app gave the patient full control of the treatment parameters, proper training to use the app was essential. In this case, the patient was an intelligent, technically savvy university student. The training included tutorial videos, help from the therapist in setting the initial parameters for treatment, the guidance of an initial 5 minute NRT treatment, and learning how to adjust the trigger during treatment. The app allowed Miley to vary the intensity of the trigger stimulus within each treatment session to maintain the desired reflex response. Based on the success of the treatment, she did this well, but many patients will likely need more support and guidance.
Reduction vs. Elimination of a Misophonic Trigger [TOP]
In this case, the NRT treatment did not eliminate the misophonic response to the trigger. At the end of treatment, Miley had no response to the recorded triggers, but she still had a weak response to the trigger in real life. This is understandable because the treatment setting was a different context than real-life, and conditioned reflexes are context sensitive (Lattal, 2012). It has been demonstrated with animal research that a conditioned reflex which is extinguished in one setting, can still occur in a different setting. The use of recorded vs. live trigger stimuli is a limitation of the NRT treatment. After the NRT treatment, sometimes a misophonic reflex will decline and extinguish in the real-life setting, and sometimes it will maintain at a substantially reduced level (Dozier, 2015a). It is also possible for the misophonic response to strengthen after treatment. If the response in real-life settings is unacceptably strong, then further counterconditioning treatments could be incorporated with a context that is closer to real life, including use of real-life trigger stimuli. In this case, at the 6-month follow-up, Miley reported that she had no trigger response to the spoon-on-bowl sounds, and a weaker trigger response to chewing sounds. It is plausible that she relaxed her hands in trigger situations, and this aided in the continued decline in her misophonic response to the treated triggers. This issue seems important when setting expectations with the patient on the goals of treatment.
Recommendations to Clinicians and Students [TOP]
This case provides support for the use of the NRT treatment for specific misophonia trigger stimuli. This treatment may be used to reduce triggers from a single source (e.g., one person) or that occur in a single context (e.g., typing at work). Triggers should be treated sequentially, using at least three different recordings of each trigger. The patient responded extraordinarily well in this case. The treatment reported in Dozier (2015a) took over 5 months, and the patient in this study also responded well. An individual who responds more slowly may require a significantly longer treatment. The NRT treatment should enhance other treatments, such as an audiologist-provided behind-the-ear sound generator or CBT therapy, because it reduces the initial physical reflex of misophonia.
Identifying the Initial Physical Reflex [TOP]
This case demonstrated the importance of identifying the initial physical misophonic reflex (see Figure 3) and addressing the reflex in treatment. The therapist should help the patient identify the physical misophonic reflex as part of the assessment, which can often be accomplished by having the patient relax while hearing a single, short, quiet trigger. In this setting, the patient can often identify a specific physical response. Rarely can a misophonic patient accurately identify their initial physical reflex prior to assessment. Typically patients have reported some of the physiological responses that accompany the extreme emotional responses of misophonia as their initial physical reflex. The author has witnessed initial physical reflexes that include virtually every skeletal muscle and many internal responses (e.g., esophagus constriction, stomach constriction, intestine constriction, sexual sensation, nausea, and the urge to urinate). Many individuals have a reflex that affects several muscles (e.g., calves and toes, shoulder and neck, or several muscles in arm).
Incorporating Applied Relaxation into the treatment protocol is highly recommended, with a focus on gaining control of the affected muscle. Prolonged use of Applied Relaxation may be critical to cases in which the treatment effect is slower.
Response to Treatment [TOP]
The NRT treatment addresses the physical reflex response of misophonia. The treatment parameters need to be set so that the patient perceives the physical response to the trigger. Some patients have reported a combined emotional and physical response using the Misophonia Trigger Tamer and have responded to treatment. Cases wherein the individual reported only an emotional response to the trigger during treatment have not shown progress.
Some patients reported a pain or sensation in the ear. This can be caused by tensor tympani syndrome which accompanies severe misophonia (Jastreboff & Jastreboff, 2014). This should be considered an accompanying symptom of misophonia and not the initial physical reflex. The settings for the trigger stimulus in NRT treatment need to be high enough to activate the initial physical reflex. Tensor tympani syndrome will likely be eliminated by successfully treating misophonia (Jastreboff & Jastreboff, 2014).
Visual Triggers [TOP]
The Misophonia Trigger Tamer app is a means of delivering the NRT treatment for auditory triggers. Visual triggers are common in misophonia and often develop to visual stimuli paired with an auditory trigger. The Visual Trigger Tamer app can be used to provide the NRT treatment for visual triggers. The app uses a video clip for the trigger and allows video, audio, and pictures to be included in the playlist.
Misophonia Severity vs. Elimination of Misophonic Reflex [TOP]
The MAQ sum score provides a measure of the distress of an individual due to misophonia. This measure seems to be sensitive to the pervasiveness of trigger stimuli for the individual, as well as the severity of the response to individual triggers. For example, one patient used white noise and open ear headphones as the sole treatment. Her MAQ sum score dropped from 47 to 17 after one assessment and management session because the noise reduced the severity of the misophonic response so she felt no anger. Treatment should include some methods of escape and avoidance of trigger stimuli to have an immediate, meaningful improvement in the distress caused by misophonia. This is likely to aid in the effectiveness of the NRT treatment because the reflex is not continually strengthened through exposure to the trigger and the patient will have an overall improvement in well-being, enabling a positive emotional state for the NRT treatment.
Talk Therapy Treatments [TOP]
Individuals often seek the help of a psychological therapist for misophonia. In such cases, the therapist should consider all component parts of the misophonic experience. As shown in Figure 5, these parts are the trigger, the physical reflex response, the emotional response including physiological arousal, and overt behavior. The causal interactions shown with horizontal lines are those observed in this case, but it is likely that, in many cases, there are more complex interactions, as shown by the dotted lines. Parents generally seek help because of problems with overt child behavior. CBT or other talk therapy is often requested. Two case studies using CBT for misophonia reported positive outcomes (Bernstein et al., 2013; McGuire et al., 2015). It is recommended that a treatment plan address all component parts. Addressing only the overt behavior with enticing rewards seems contraindicated.
Misophonia and Sensory Processing Disorder [TOP]
Sensory processing disorder (SPD) or sensory over-responsivity shares similarities of symptomology with misophonia, and it has been suggested that SPD and misophonia are manifestations of a single disorder (Taylor et al., 2014). SPD manifests as over or under-responsiveness to stimulation from touch, taste, smell, vision, hearing, and movement, with tactile and auditory sensitivity being the most common (Reynolds & Lane, 2008; Taylor et al., 2014); and SPD auditory sensitivity is primarily to unexpected and loud noises (Schröder et al., 2013). Misophonia is generally limited to low volume auditory stimuli and visual stimuli associated with the auditory stimuli or repetitive movements. Therefore, SPD and misophonia can be viewed as different, unassociated conditions which may both result in an anger or fight-flight response (Schröder et al., 2013). Furthermore, we view the physical misophonia muscle reflex to trigger stimuli as additional support that SPD and misophonia area distinctively unique and different disorders.
Conclusion [TOP]
Misophonia is a relatively unknown condition that is a detriment or impediment to the lives of many individuals. Although many think of misophonia as a rare disorder it may afflict hundreds of millions individuals worldwide. There is a great need for fundamental research on misophonia as well as research to validate assessment instruments and establish empirically-validated treatments (Webber & Storch, 2015). Misophonia research seems to be limited by a lack of interested professors and by institutes who have committed research tracks for various neurological and psychological conditions.
In this case, the debilitating effects of misophonia were ameliorated by treating a conditioned muscle reflex response to specific misophonic trigger stimuli and by the patient developing a generalized response of relaxing muscles when triggered. Although the patient experienced misophonia as an extreme emotional responses to specific environmental stimuli, it appears that her condition would be more accurately described as a conditioned skeletal muscle reflex response to specific environmental stimuli which in turn elicited extreme emotional responses. Likewise with the naming of this condition, misophonia focuses on the emotions of this disorder and diverts attention form a core component of the disorder, which is a conditioned aversive reflex. Further research on the components of misophonia is warranted. Aversive stimuli have been shown to evoke fight-or-flight responses in humans (Berkowitz, 1983; Berkowitz, Cochran, & Embree, 1981). These studies found that the aversive stimuli evoked a range of emotions that may not be reflected in overt behavior. Other research identified activation of the limbic system of humans in response to aversive odorants (Zald & Pardo, 1997) and to aversive gustatory stimuli (Zald, Lee, Fluegel, & Pardo, 1998). Such responses seem consistent with those of individuals with misophonia.
Some individuals with misophonia have a weak physical reflex. In these cases, the physical stimulus is too mild to be comparable to aversive stimuli used in research studies; however, the stimulation of the physical reflex may elicit a conditioned emotional reflex. The physical reflex is intrusive, and difficult to not perceive. A person may apply distraction techniques to divert their focus from the trigger stimuli, but the physical stimulation is still perceived and could therefore elicit the conditioned emotional response. For these reasons, a more appropriate name for Misophonia would be Conditioned Aversive Reflex Disorder.
Misophonia is generally viewed as a life-long, debilitating condition, which is disruptive to social and professional life, and becomes progressively worse with time. This case study treatment provides some encouraging results where the typical course of this condition was potentially reversed and apparently abated. It is hoped that the information presented here can supplement other work in developing treatment for misophonia to provide meaningful relief to those suffering from this disorder.

 This is an open access article distributed under the terms of the Creative Commons
Attribution License (
This is an open access article distributed under the terms of the Creative Commons
Attribution License (