Introduction [TOP]
Background [TOP]
The concept of Multidisciplinary teams (MDTs) are a well-known way of working which sees both health professionals across the disciplines integrating in their work and approaches when considering collaboratively an individual treatment plan for a range of clients. An MDT is formed by professionals from the healthcare field and allied disciplines who are seen as collaborating in the formulation of recommendations that aims to facilitate the quality of provision-care for clients (Department of Health, 2015; Mental Health Commission, 2006). According to Moss (1994) within Mental Health provisions, multidisciplinary teams enable three key functions: a) continuing proactive care for those affected by long-term mental health issues, b) 24/7 care during support, intervention and treatment before and during potential crisis, and c) organised responses to requests for care. As the definition highlights, multidisciplinary teams seek to enrich the understanding of the client and the context in which the client operates/functions by integrating, and interrelating different perspectives to the formulation of a client’s case with the common aim and goal of a comprehensive programme and treatment plan to the issues presented. The specificity of multidisciplinary teams lies on the enriched understanding of an issue which stems from different disciplines and aims, with their specialities and expertise, to come together towards a common treatment and resolution to the issue. Professionals designated to MDTs can stem from a range of disciplines from the health care professions and can include practitioner psychologists, speech and language therapists, occupational therapists, psychiatrists, specialist nurses, physiotherapists, nutritionists; and the list is not exhaustive. Within sport and science teams it can also include sport scientists, masseurs and personal trainers as well as medical doctors. The richness of their knowledge and expertise, through assessments, design, delivery, monitoring and evaluations of programmes, aims to provide a person-centred plan which holistically can suggest treatments to resolve experienced issues.
Despite some critique on the actual effectiveness and challenges for resource allocations (Ke et al., 2013), multidisciplinary teams have been part of the health and social care industry for a number of years and very much have risen from a move towards a more person/client centeredness way of working, where the main drivers for success have been identified as collaboration and co-operation in the pursuit of a common clear aim (Barr, Hammick, Koppel, & Reeves, 1999). Whilst the client/person sits at the centre, multidisciplinary teams assess, design, deliver and monitor plans and interventions for the benefit of the client/person. This climate of collaboration and co-operation needs however to be actively pursued, there where often conflicts and competition present as potential barriers. Ke et al. (2013) in their systematic review of multidisciplinary effectiveness have also suggested that multidisciplinary teams work demands considerable organisational, management and funding in order to secure that relevant professionals can actually attend, that key client’s information is collected, and ultimately that all information is discussed by the specialist professionals throughout this process. In order to better understand multidisciplinary teams work and its potential barriers, a better definition and understanding of these risks need to be explored and understood. By better understanding these barriers, it is hoped that associated resolutions can be shared for more effective MDTs work.
The study of human and social psychology can shed light on the characteristics of both individuals and group dynamics which can be very useful in better understanding how multidisciplinary teams work. Clark (1993) suggests that placing people together coming from different disciplines, it is not a guarantee for the emergence of shared understanding. The nature of conflicts can often be experienced by members of the group in a personal and quite idiosyncratic manner, often differently experienced depending on particular professionals involved and/or the nature of the issue to be addressed. Whilst general conflict is recognised as a potential universal barrier, it is more the quality of the experienced conflict that can determine (or not) successful collaboration. Indeed research suggests that a level of healthy conflict is necessary in keeping MDTs alive. It is also considered a key element in the process towards positive change and subsequently growth and rejuvenation (Berg-Cross, 2000; Brown, 2000). This paper aims to clarify these barriers by reflecting on the author’s personal experiences in working with a number of multidisciplinary teams where location, time, resources, communication, level of expertise can all give rise to multiple interpretations of key definitions and can shape a number of potential idiosyncratic barriers whilst trying to achieve a desired positive common outcome.
Method [TOP]
Reflections were collated and formulated by the author through reflective personal notes/diary from attendance to a number of professional review meetings involving various professionals from Education, Health and Social Services from over 15 Local Authorities in UK and associated CAMHS services. In addition, reflective notes were collated through working experiences from in-house services through bi-monthly multidisciplinary meetings over a period of over twenty-four months which included professionals from psychology, speech and language therapists, occupational therapists, lead teachers, specialist behavioural nurses, psychiatrists and social workers. A qualitative thematic analysis of this data and reflections was carried out in order to identify relevant factors characteristic of MDT work. These factors were then clustered under main themes. These are discussed in the next sections.
Results [TOP]
Identified Risk Factors: Inhibitors, Conflicts and Boundaries [TOP]
Conflicts can take place between individuals, between the individual and the team and also between teams. Multidisciplinary work and approaches are fertile areas for these types of conflict to emerge (Reid, Stewart, & Thorne, 2004). Pirrie et al. (1998) in their work on multidisciplinary learning within health care teams on their first year course suggest that specific professional groups were expressing concerns related to a lack of opportunities to consolidate their professional identity within their own discipline. Issues of professional boundaries can stem when a number of professionals from different disciplines come together; boundaries that are both usually defiantly protected and yet in need to be permeable and flexible for a multidisciplinary team work to be successful. It is not unusual for different practitioners within the same discipline to significantly differ in their approaches and treatment plans (Reid et al., 2004).
In addition, practitioners are charged with integrating advice from different disciplines, but often have their own philosophies and opinions which have stemmed from a wide range of experiences that undoubtedly will, at some point, affect their decision making process and subsequent practices. A barrier that emerged from the analysis and not to be underestimated is the complexity of the context and ‘organisms’ of which the client is part of, namely his/her family and extended family members, carers/guardians and larger organisations such as those who are responsible for funding the placements and provide support. Often un-clarity of who is doing what, or who is responsible for what, or perceived to be responsible for, can cause significant amount of conflict and even resentment; resentment for not reaching timely results or resentment towards the system. These risk factors are discussed in more details in the next section, with a discussion and reflection on the following themes: 1) communication barriers, 2) resources, 3) size and 4) ambiguity and interdependence.
Communication Barriers: What and How We Communicate [TOP]
This risk factor has been identified as significantly compounding to the sense of conflict, and tension that is often characteristic of multidisciplinary teams. It can stem from a variety of sources including personal and professional differences, differences in knowledge base and very much isolated to each discipline, either sporadic team meetings or meetings where not all professionals are actively and openly participating in constructive discussions, analysis and reflections.
Communication barriers can stem from a lack of shared and clear aim and where personal goals in promoting each professional discipline and individual perspectives become the priority. Rather than focusing on the person/client centeredness and related needs, the focus can at times quickly shift to the individual professional perspectives. Often a common feature of experts is their confidence in their opinion/approach stemmed from a longstanding working/practice experience, training and knowledge (Reid et al., 2004). This confidence can often leave little space for the acceptance of others' opinions and more generally for constructive conflict resolutions. Interestingly though, whilst cohesion can lead to better productivity, satisfaction and decision making, it is also suggested that within multidisciplinary sport group dynamics, conflict conditions do not necessarily equate to under-performing (Lenk, 1969). Therefore rather than cohesion, we can talk of homogeneity and heterogeneity. Both will be explored further as part of key success factors.
Communication barriers can also be experienced when the client and his/her family members become (as best practice suggest) the centre of these discussions. Conflict conditions arising from multidisciplinary teams can often significantly displace the trust of the client and its family members, translated into us and them rather than a team working together for and more importantly towards a common purpose where the client sits at the centre. Family members and carers are also individuals with their own opinions and experiences which can yet add another dimension to the potential conflict and misunderstanding.
Communication barriers are manifested by often an inability to openly listen to other professionals’ perspective and an inability to willingly tolerate and trust each other’s perspective in the pursuit of a common goal/aim which clearly needs to be defined at the onset. Furthermore, language used by professionals can have its own syntax and definitions which are closed to the particular professional group in question. On the surfaces this phenomenon can be underestimated whilst in effect it can lead to a number of misinterpretations and confusion. Perhaps the lack of this clarity at the start is what needs to be better clarified and agreed.
Another risk which emerged from the author’s reflections is known as triangulation, alliances and coalitions. There might be instances, where in order to deflect conflict amongst professionals and clients, alliances are formed between two or more people against others, so as to create ‘partners in action’ whilst it only creates an atmosphere of conflict and alienation. In fast changing dynamic groups of professionals stemming from different but converging disciplines, these potential barriers need to be addressed with skilful negotiation, so as to ensure that no members of the group are feeling ‘left out’ but that true collaboration and co-operation is nurtured.
Resources: Accessibility and Availability [TOP]
This is another potential source for conflict which emerged from reflection and analysis and encountered within multidisciplinary teams. Current financial hardships have significantly streamlined services where often long waiting lists have become the norm rather than the exception. When experts are consulted, they are often limited by the resources available and allocated to them, fragmented working patterns – often employed on a part-time basis – or subject to a high proportion of staff turnover and fragmented service provisions, which as a result, can lead to communication difficulties. Key information has not been passed on, or in worse cases, it has been missed altogether. The information sharing process is key, but this again requires a certain level of resources which need to be timely accessible.
Size: How Many Members? [TOP]
Group size is a well-known factor in social science to be contributing to conflicts. As the size of the membership increases so is the shifting of responsibility and as a consequence, group productivity. Members of the group may increasingly feel invisible and de-personalised leading to a known phenomenon called social loafing (Karau & Williams, 1993). Furthermore, when more than one professional works within the same discipline, potential issues of boundaries and territory can ensue where members of the group may feel threading on each others with a growing result of lack of clarity and productivity. Through the analysis the size of MDTs seemed to be a significant contributing factor to the success of intervention/plan. The absence of a lead professional within MDTs was also observed in some cases to be an important critical factor for success. And sometimes the unwillingness to embrace and accept a lead professional from a different discipline or the lack of training necessary to ensure this type of work and approach could lead to challenges. The larger the groups are and the smarter and tighter organisational dynamics need to be so as to ensure that productive work gets completed and where conflicts of opinion arise, they can get timely treated and resolved in the best interest of the client.
Accountability: Ambiguity and Interdependence [TOP]
When a number of professionals from different disciplines are assessing the issues at stake in order to provide an intervention or strategy as part of a package, often the context and historical information may not be in line with current thinking and practice. This can easily lead to conflicts of interpretation of the issue and as a result conflicts on the appropriate approach and solution. With this rising ambiguity professionals can either feel devalued or take a more rigid stance where only one solution is embraced: usually their own. This can often lead to feelings of resentment and frustration which are very easily transferred to staff and teams, family members, other carers – and ultimately the client – who may be in need of receiving supportive training in a specific intervention. Ultimately, this sense of frustration and disempowerment leads to a level of ambiguity and eventually to ineffective interventions. And with ambiguity and ineffective interventions comes the lack of self-belief that an intervention is going to be effective in the first place even before it has been fully implemented. On the other hand, situations have risen, where ambiguity is a product of interdependence between different professionals and their disciplines, where lack of clarity of roles – who will be the person taking the lead in a large group of people – and where assumptions of specific roles taken can become fuzzy. These systemic challenges can all lead to conflicts and potentially to fatal flaws or – in best instances – to very ineffective and costly interventions. There are potentially a number of key factors that can affect the effectiveness of multidisciplinary teams work; sometimes the sheer number of risks factors can compound to the failure of interventions and at times to the breakdown or the premature suspension of support provided as a result of their ineffectiveness.
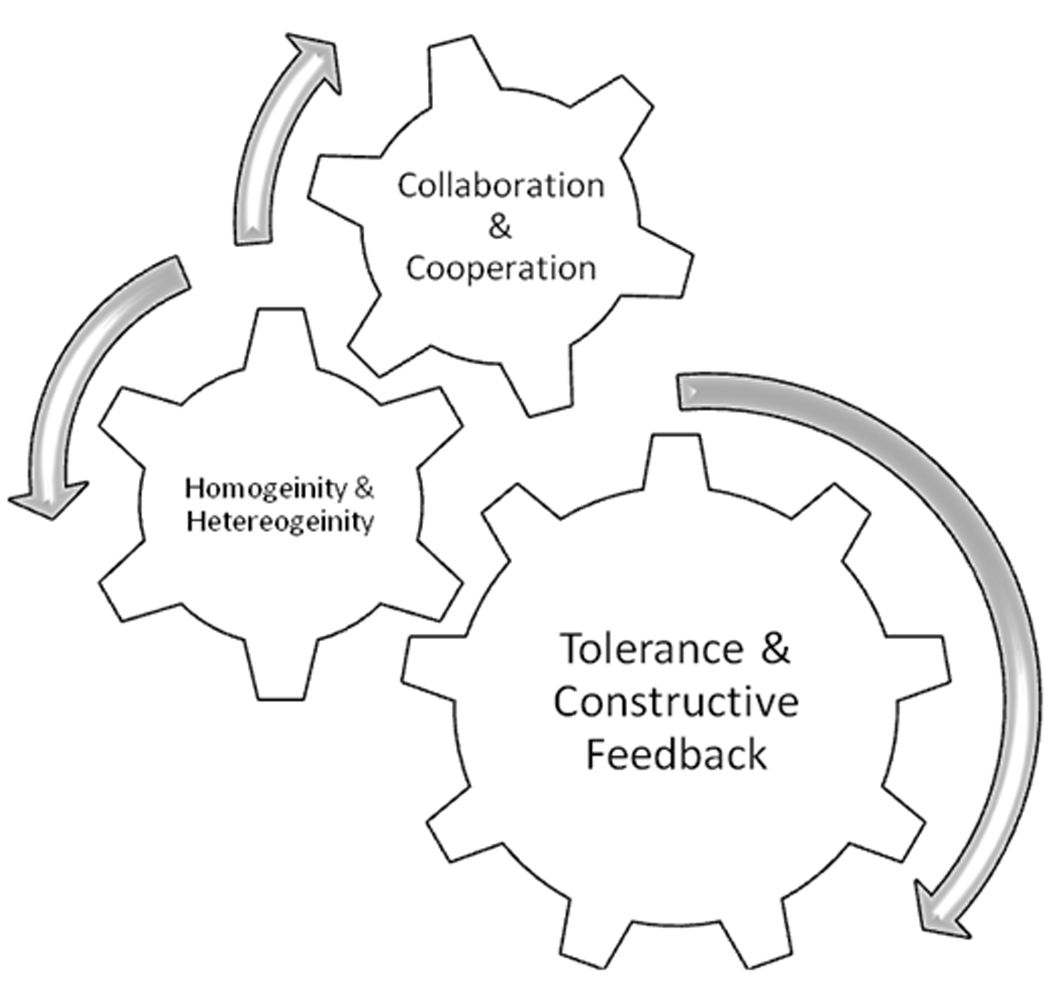
The MDTs intervention has not been adopted for long enough time to be able with evidence and certainty to conclude that it has been unsuccessful. At times it is just the sheer number of ‘changes’ and ‘transitional points’ which contribute to a fragmented and vulnerable MDT, at other times corrective actions become the focus of the multidisciplinary team work which takes away energy, focus and indeed productivity from the actual original goal and aim: the needs of the client. A useful way of addressing and better understanding the dynamics of MDTs work according to the analysis presented is to reflect on factors which actually have contributed to its success. Key elements have been selected, for the purpose of this discussion and these are as follow: a) role of multidisciplinary teams – clarity; b) collaboration and co-operation c) identified qualities: homogeneity vs. heterogeneity and d) tolerance and constructive feedback – constructive criticism.
Figure 1 aims to highlight some emerging key elements which have been identified for desired outcomes. They will be discussed in the last section.
Discussion [TOP]
Multidisciplinary Teams: Clarity of Roles [TOP]
Given the above reflections so far presented and the potential identified barriers and risks factors, a summary of key elements resulting from the author’s perspective, which can potentially contribute to successful multidisciplinary team work, will now be discussed. As Nolan (1995) put it: (Inter) (multi) disciplinary care, although not denying the importance of specific skills, seeks to blur professional boundaries and requires trust, tolerance, and a willingness to share responsibility (p. 306). Similarly the author’s reflections presented in this article suggest that multidisciplinary teams work requires a level of established trust in each other competencies, a level of tolerance in embracing one other’s perspectives and more importantly a willingness to share roles and responsibilities after a clear, well-defined and agreed shared aim/goal. Perhaps the initial question to be asked when multidisciplinary teams are formed together is indeed ‘what is the role of this multidisciplinary team and its aim/s?’ ‘Who is putting together this multidisciplinary team?’ Once these initial questions are actually addressed and a common answer agreed, it is suggested that it is about exploring flexibility within the well-defined structure of the team which can promote change, collaboration and co-operation.
Collaboration and Co-Operation: What Does It all Mean? [TOP]
A definition of co-operation from the Oxford Dictionary states that it is ‘the action or process of working together to the same end' (Oxford Dictionary, 2015). True collaboration and co-operation requires therefore shared aims, shared value systems and honest, respectful and purposeful communication: all themes which have emerged from the author’s analysis of data.
In order to address barriers of alliances and triangulation previously discussed, opportunities for negotiation and clarification need to be purposefully fostered through trustful partnership. In order to realise shared goals, a sound collective commitment is required and before this, a clear understanding of what type of information is shared, with who and in what time frame. Self-reflections have also highlighted that these stages can be often overridden by an overreliance on the desire to ‘get to the end’ especially when resources are constrained and people experience uncertainties in their roles/jobs. This means that often the actual process is overshadowed by the emergency of an immediate plan. This immediacy can often risk of being ineffective.
Identified Qualities: Homogeneity and Heterogeneity [TOP]
In order to achieve a level of solidity within a multidisciplinary team which is necessary in order to avoid fragmentation and potential unhealthy alliances, homogeneity has emerged from the author’s reflections as an important key element for success. However, this homogeneity needs to be balanced with a level of heterogeneity which can add a level of healthy tension where a level of threat can encourage cohesion in a group. Reaching this balance between homogeneity and heterogeneity within a MDT requires skilful interpretations of potentially sensitive situations and the ability to adjust accordingly to its different manifestations. In the discussion paper from the Mental Health Commission (2006) it is suggested that in order to nurture key competencies towards MDT, some consideration needs to be addressed at a training level, through both professional courses at undergraduate and post-graduate levels. This process will partly address some of the competencies necessary for effective MDT work. And in the absence of this initial training, opportunities for developing these competencies need to be offered at the start of any MDT work.
Conclusions [TOP]
Maintaining the Health of a Multidisciplinary Team [TOP]
In order to better understand multidisciplinary team work, this paper presented some reflections from the author’s perspective, on the risks and barriers encountered through this model of working which has been driven in the last 10 years within health, care, education and sport. It tried to better define emerging risk factors stemming from the author’s own working experiences. Themes were identified throughout the analysis and these were presented and discussed. What the analysis suggested is that risk factors can often lead to ineffective and costly interventions. Furthermore, as a result of these reflections, the paper aimed to identify and highlight key elements for successful multidisciplinary team work and to present critical key success factors. It is suggested that these critical key factors need to be positive drivers through a continuous process of integration, collaboration and co-operation. In summary these key success factors can be defined as follow:
-
The importance of setting right at the start of any MDT work clarity in roles. As highlighted in a discussion paper from the Mental Health Commission (2006) this will identify clearly what professionals need to have and what they need to achieve within the workplace.
-
The importance of nurturing MDT work through setting out clear values, attitudes and teams’ knowledge.
-
The importance of establishing right at the onset of multidisciplinary team work a shared and committed aim where everyone, though rising from different disciplines, competencies and capabilities are all truly in agreement and committed to adhere to and work towards.
-
The importance of establishing a level of trust and tolerance in the pursuit of true collaboration and co-operation. This will undeniably include misunderstanding, a level of conflict and personal and professional differences which need to be seen as generating creative thinking, partnership and ultimately effective solutions.
-
The importance of accepting change within a homogeneous team who still works towards a common and agreed goal.
-
The importance of acknowledging differences in communication styles which (regardless) need to be open, transparent, respectful and effective.
-
The importance in addressing concerns and ambiguities through collaborative opportunities to discuss and openly and constructively seek and provide immediate but also long-term corrective treatments.
-
The importance of recognising (and tolerating) that an individual perspective can at times be overridden there where an individual opinion might not at the time be the most effective and might not reflect a more general commitment to treat the identified risk.
-
Acknowledging and accepting feedback constructively will remain a key success factor in the maintenance of a healthy multidisciplinary team work.
-
The importance to recognise a component of MDT which highlights reflective practice in action and a commitment to working with new and changing models of education, health and care for life-long learning.
Having highlighted these emerging key success factors stemming from the author’s perspective, it is hoped that further and more frequent practitioners’ reflections can be shared in the future on the topic of multidisciplinary team work. The aimed benefits of hopefully improving our local and national services, where the skilful knowledge from different disciplines and perspectives are truly integrated together will continue to provide more enriched, efficient and effective care, education and health to a range of clients, their families and organisations as a whole.

 Contents
Contents This is an open access article distributed under the terms of the Creative Commons
Attribution License (
This is an open access article distributed under the terms of the Creative Commons
Attribution License (