The interest in finding factors related to the presence of mental health is mostly driven by the possibility of interventions in terms of prevention and promotion of health. The aim is to identify which variables function as risk or protective factors of mental health. Because the development of psychology as a science has been mainly guided by the medical model, whereby mental health is the absence of pathology (Millon, 1996), the progress in psychology has been focused mainly on diagnosing and treating mental disorders. However, the absence of psychological symptoms does not guarantee the presence of mental health, especially in terms of quality of life and optimal functioning (Seligman & Csikszentmihalyi, 2014; World Health Organization, 2014). Therefore, research aimed at describing mental health and identifying factors related to its presence should study mental health as a whole. To do this, analyses should include the study of psychopathological symptoms and well-being signs conjointly, that is, research should encompass the complete state of mental health.
Complete Mental Health [TOP]
A proposal comprising mental health as a whole was postulated by Greenspoon and Saklofske (2001): the Dual-Factor Model (DFM). This model departs from the claim that a decrease in symptomatology does not necessarily imply an increment in well-being and vice versa. The DFM proposes a combined assessment of both aspects given by four possible scenarios: (1) subjects with low symptomatology and low well-being; (2) subjects with high symptomatology and low well-being; (3) subjects with low symptomatology and high well-being; and (4) subjects with high symptomatology and high well-being. Following Suldo and Shaffer (2008), these groups may be labelled (1) vulnerable, (2) troubled, (3) complete mental health–also called flourishing (Kelly, Hills, Huebner, & McQuillin, 2012) – and (4) symptomatic but content – also labelled ambivalent (Eklund, Dowdy, Jones, & Furlong, 2010).
A similar model was developed by Keyes (2005): the Complete State Model of Health. This author proposes that health and sickness are two correlated unipolar dimensions that together constitute a complete state of mental health. Keyes (2005) conceives mental health as a state of flourishing in which individuals do not exhibit psychopathology and have signs of well-being. By contrast, a state of languishing refers to the individuals who have a high level of psychopathology and a low level of well-being. All other subjects that do not fit into these two categories are considered to be in a moderate state of mental health. Research that incorporated this methodology evidenced the importance of analysing symptoms and well-being together (e.g. Góngora & Castro Solano, 2017).
It has been found that individuals who present complete mental health are less likely to have a cardiovascular disease (Keyes, 2004) and report having better physical health (Suldo & Shaffer, 2008), better academic achievement (Antaramian, 2015; Antaramian, Huebner, Hills, & Valois, 2010; Guerra Vargas, 2017; Lyons, Huebner, & Hills, 2013; Suldo & Shaffer, 2008; Suldo, Thalji, & Ferron, 2011), fewer behaviour problems (Eklund et al., 2010), more hope and gratitude (Eklund et al., 2010) and less internalising behaviour (Smith, 2018). Although the greatest contrasts in these findings are mostly between the complete mental health group and the troubled group, Antaramian et al. (2010) stated that the vulnerable group–characterised by low symptomatology and low well-being–was as likely to have low academic achievement and to exhibit problematic behaviour as the troubled group. Among the investigations on the DFM, Trompetter, Lamers, Westerhof, Fledderus, and Bohlmeijer’s (2017) research is interesting since they concluded that it is fundamental to measure progress in psychotherapy from a DFM perspective.
Different variables have been found to affect the state of complete mental health as conceived by the DFM. Social support, for example, has been reported to positively influence the presence of complete mental health (Kelly et al., 2012; Magalhães & Calheiros, 2017). Concerning personality traits, different studies using the Five Factor Model (FFM; Costa & McCrae, 1985) classification concluded that neuroticism increases the odds of belonging to the troubled, symptomatic but content and vulnerable groups and that extraversion increases the odds of belonging to the complete mental health group (Lyons, Huebner, Hills, & Shinkareva, 2012; MacMahan, 2013). The relative novelty of the DMF lies in the little empirical evidence of the association between personality traits and complete mental health. As personality traits are characterised as consistent patterns of behaviour, emotion and thought that are relatively stable over time and identifiable in different contexts (e.g., Allport, 1937; Cattell, 1965), they are central aspects of any individual and, therefore, determine many of his or her experiences. The state of complete mental health should not be an exception.
Positive Personality Model: Positive Personality Traits [TOP]
De la Iglesia and Castro Solano (2018) have recently postulated a new personality trait model that assesses traits in their positive versions: the Positive Personality Model (PPM). This sanity model is associated with the pathological traits model proposed in Section III of the Diagnostic and Statistical Manual of Mental Disorders in its fifth edition (DSM-5; American Psychiatric Association, 2013) as well the FFM (Costa & McCrae, 1985). The PPM constitutes a positive pole in the personality traits continuum, completing the notion of dimensional continuity in the study of personality traits (e.g., Leary, 1957; Millon, 1996; Millon & Everly, 1994; Offer & Sabshin, 1991; Strack & Lorr, 1994).
The availability of a conceptual framework that integrates pathological and normal classifications has generated an increased interest in the scientific community and applied fields (e.g. Huppert & So, 2013; Leising, Rogers, & Ostner, 2009). The positive traits that make up the PPM are as follows: serenity (negative affectivity in the pathological version and emotional stability in the FFM), characterised by an almost imperturbable state of peace and calmness; humanity (detachment in the pathological version and extraversion in the FFM), implying a high contextual sensitivity and an orientation towards others in terms of solidarity and assistance; integrity (antagonism in the pathological version and agreeableness in the FFM), characterised by trust, honesty and humility; moderation (disinhibition in the pathological version and responsibility in the FFM), implying caution and reflection before action; and lastly, sprightliness (psychoticism in the pathological version and openness to experience in the FFM), related to having self-confidence and clear goals, being active and feeling satisfied. The ultimate aim of the PPM is to function as a sanity nosology that is updated and integrated into the latest notions in personality diagnosis.
The PPM has been empirically supported by the validation of its measurement instrument and other studies. Results showed that the positive traits are positively and partially related to FFM traits and negatively related to DSM-5 pathological traits. These relations place PPM traits in the positive pole of the traits’ continuum. Additionally, when compared to normal traits (e.g. FFM), PPM positive traits showed evidence of incremental validity because they performed as better predictors of positive mental health in the general population (de la Iglesia & Castro Solano, 2018), of job performance and satisfaction (de la Iglesia, Lupano Perugini, & Castro Solano, 2019) and of academic adjustment and achievement (de la Iglesia & Castro Solano, 2019) .
This research aimed at analysing PPM positive traits in relation to the DFM. The specific objectives were (a) to determine whether the positive personality traits are related to psychological symptoms and well-being; (b) to investigate whether the presence of positive traits differs across the different groups configured according to the DFM; and (c) to test the predictive power of PPM positive traits in the odds of belonging to the DFM groups.
Method [TOP]
Participants [TOP]
The sample was composed of 1502 Argentinean adults from the general population. The mean age was 39.79 (SD = 14.23, Min = 18, Max = 83, 50.1% male, 49.9% female). Most of them (66.5%) lived in Buenos Aires City, 26.4% (n = 396) in the greater metropolitan area of Buenos Aires City, and 7.1% in some of the country’s provinces. As for their maximum educational level, 7.3% of the participants had not completed high-school, 14.7% had finished high-school, 35.3% were attending college, 35.5% (n = 533) had completed college, 2.1% (n = 31) were attending a postgraduate course and 5.1% had obtained a postgraduate degree. With respect to their socioeconomic status (SES), most participants (67.8%) reported middle SES, 20.3% upper-middle SES, 10.3% lower-middle SES, 0.9% high SES and 0.8% low SES.
Materials [TOP]
Positive Traits Inventory–5 [TOP]
The Positive Traits Inventory–5 (PTI-5; de la Iglesia & Castro Solano, 2018) is a positive personality traits measure composed of 60 items that are answered in a six-point Likert-type scale ranging from 0 (completely false) to 6 (completely true). This test is a positive reverse version of the Personality Inventory for DSM-5 - Adult (PID-5; Krueger, Derringer, Markon, Watson, & Skodol, 2012), a scale of pathological traits included in DSM-5 (American Psychiatric Association, 2013). The positive traits assessed are sprightliness (17 items), integrity (13 items), serenity (13 items), humanity (8 items) and moderation (9 items). PTI-5 has sound psychometric properties regarding its factorial structure and internal consistency. In this sample, Cronbach’s alpha was as follows: sprightliness α = .90, integrity α = .85, serenity α = .88, humanity α = .80 and moderation α = .84.
Symptom Checklist 90 Revised [TOP]
The Symptom Checklist 90 Revised (SCL-90-R; Derogatis, 1977), a 90-item scale, is used to measure the presence of psychological symptoms in the past seven days. The respondent is asked to indicate how much he or she was bothered by a number of symptoms on a five-point Likert scale (1 = not at all to 5 = extremely). It has nine subscales, but in this study only the Global Severity Index was used. This measure informs about the general psychological distress of the individual assessed. Psychometric studies in the Argentinean population have shown good psychometric properties (Casullo & Castro Solano, 1999; Sánchez & Ledesma, 2009). In this study, the internal consistency measured by Cronbach’s alpha was .97.
Mental Health Continuum–Short Form [TOP]
The Mental Health Continuum–Short Form (MHC-SF; Keyes, 2005) is a 14-item measure of well-being. Three subscales can be assessed: emotional, psychological and social. It uses a six-point Likert scale based on how often the respondent has felt different well-being states (0 = never to 5 = everyday). Its factorial structure was confirmed in its local adaptation, where evidence of convergent validity was also obtained (Lupano Perugini, de la Iglesia, Castro Solano, & Keyes, 2017). Cronbach’s alpha for the total score in this sample was .88.
Results [TOP]
Associations Among Positive Traits, Psychological Symptoms and Well-Being [TOP]
Product-moment Pearson correlations were calculated in order to explore the associations between PPM positive traits and the presence of psychological symptoms and well-being. In the global severity index–a measure of psychological symptoms–all correlations were statistically significant and negative (p < .01). The strongest association was with sprightliness, r(1500) = -.47, p < .01. Moderate associations were found with serenity, r(1500) = -.34, p < .01, and moderation, r(1500) = -.24, p < .01, while the association with integrity, r(1500) = -.19, p < .01 and humanity r(1500) = -.14, p < .01 was weak. Regarding well-being, all associations with PPM positive traits were statistically significant and positive (p < .01). Again, the strongest correlation was observed for sprightliness, r(1500) = .52, p < .01. The associations with serenity, r(1500) = .35, p < .01, moderation, r(1500) = .20, p < .01, integrity, r(1500) = .29, p < .01 and humanity, r(1500) = .21, p < .01 were all moderate.
DFM Clusters: Differences in Positive Traits [TOP]
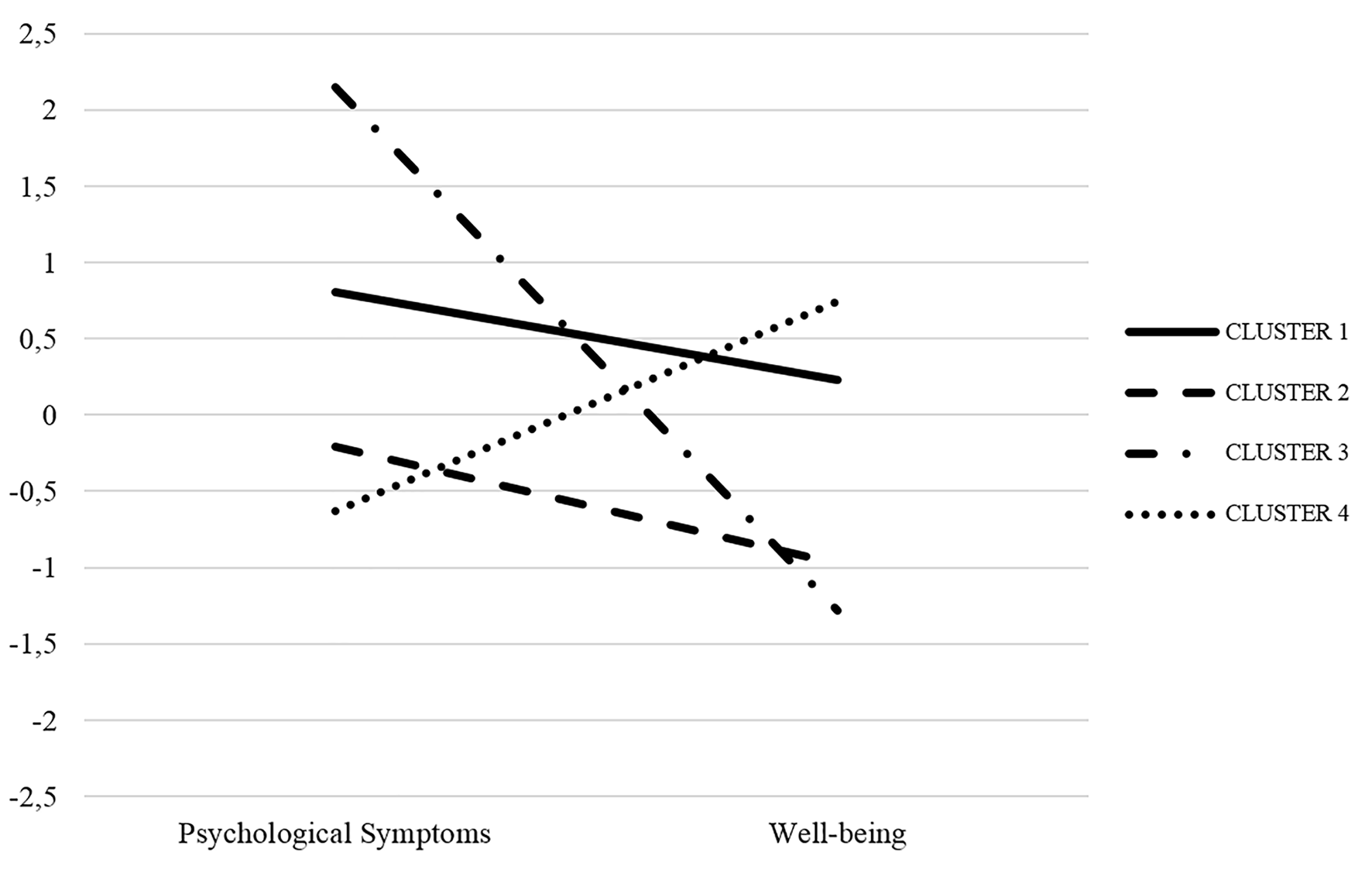
A hierarchical cluster analysis was used to identify groups according to DFM (combination of psychological symptoms and well-being). The method of choice was Ward, and the squared Euclidean distance was used to determine the adequate number of clusters that maximised the between-groups difference and minimised the within-groups difference. The conglomerate coefficient and the dendrogram suggested that a four-group solution was appropriate.
Then, four groups were classified in the k means cluster analysis. The ANOVAs showed that statistically significant differences existed in the presence of psychological symptoms and well-being regarding the cluster (p < .01). Table 1 includes the means for the presence of psychological symptoms (SCL-90-R’s global severity index) and well-being (MHC’s total score) for each cluster. It may be observed that cluster 1 scored high on psychological symptoms and well-being, corresponding to the symptomatic but content group. Cluster 2 scored low on psychological symptoms and well-being, corresponding to the vulnerable group. Cluster 3 scored high on psychological symptoms and low on well-being, corresponding to the troubled group. And finally, cluster 4 scored low on psychological symptoms and high on well-being, corresponding to the complete mental health group (see also Figure 1).
Then, a MANOVA was run to compare the presence of positive traits in DFM clusters (Table 2). Statistically significant differences were found in all positive traits regarding the cluster, Wilks' λ = .677, F(15, 4124.67) = 41.698, p < .001, η2 = .12. Post-hoc Bonferroni tests showed that individuals grouped in the complete mental health cluster had higher sprightliness, integrity, serenity and moderation. The cluster with the lowest presence of these traits was the troubled cluster. As for humanity, the complete mental health and symptomatic but content clusters had a higher presence of this trait than those who belonged to the troubled and vulnerable clusters.
Table 2
Dual Factor Model Clusters: Differences in Positive Traits
| PPM trait | Cluster
|
F | p | η2 | |||
|---|---|---|---|---|---|---|---|
| 1 (n = 241) | 2 (n = 419) | 3 (n = 153) | 4 (n = 689) | ||||
| Sprightliness | 3.68b | 3.54c | 3.03d | 4.07a | 191.25 | < .001 | .27 |
| Integrity | 4.12b | 3.97c | 3.82d | 4.24a | 33.39 | < .001 | .06 |
| Serenity | 3.22b | 3.26b | 2.87c | 3.70a | 77.75 | < .001 | .13 |
| Moderation | 3.43b | 3.46b | 3.16c | 3.71a | 28.91 | < .001 | .05 |
| Humanity | 3.77a | 3.42b | 3.37b | 3.82a | 36.99 | < .001 | .06 |
Note. Different letters indicate statistically significant differences between groups.
Prediction of the Odds of Belonging to the DFM Cluster and Precision in the Classification [TOP]
Following the analysis strategy of Lyons et al. (2012), a multinomial logistic regression was calculated to determine whether there were statistically significant changes in the odds of belonging to one cluster in comparison to another. In all cases, the comparison was with the complete mental health cluster as follows: (1) complete mental health versus symptomatic but content, (2) complete mental health versus vulnerable, (3) complete mental health versus troubled.
The model was statistically significant and showed a good overall fit, χ2(15) = 567.01, p < .001, Cox-Snell R2 = .314. All positive traits, except for moderation (p > .05), were statistically significant predictors (p < .01). Table 3 displays the estimated parameters for each comparison. In the comparison with the symptomatic but content cluster, sprightliness and serenity increased the odds of belonging to the complete mental health group, whereas integrity and humanity decreased these odds. The same pattern was observed in the comparison with the vulnerable cluster. Finally, in the comparison with the troubled cluster, sprightliness was the positive trait that increased the odds of belonging to the complete mental health cluster and integrity was the one that decreased these odds. The percentage of correct classification was 55%, that is, the model was able to predict the odds of belonging to one of the DMF clusters with a significance level better than chance (c-statistic = .688, p < .05).
Table 3
Model Parameters of the Multinomial Logistic Regression: Predictive Model of DFM Clusters by PPM Traits
| PPM trait | B (SE) | 95% CI OR
|
||
|---|---|---|---|---|
| LL | OR | UL | ||
| Symptomatic but content vs. Complete Mental Health | ||||
| Intercept | 3.68 (0.70) | |||
| Sprightliness | -1.61 (0.19)** | 0.13 | 0.19 | 0.29 |
| Integrity | 0.68 (0.19)** | 1.36 | 1.98 | 2.89 |
| Serenity | -0.71 (0.12)** | 0.38 | 0.48 | 0.63 |
| Moderation | -0.09 (0.12) | 0.71 | 0.91 | 1.16 |
| Humanity | 0.39 (0.13)** | 1.12 | 1.47 | 1.93 |
| Vulnerable vs. Complete Mental Health | ||||
| Intercept | 6.53 (0.60) | |||
| Sprightliness | -1.92 (0.17)** | 0.10 | 0.14 | 0.20 |
| Integrity | 0.58 (0.16)** | 1.30 | 1.80 | 2.47 |
| Serenity | -0.41 (0.11)** | 0.52 | 0.66 | 0.83 |
| Moderation | 0.17 (0.11) | 0.96 | 1.19 | 1.47 |
| Humanity | -0.35 (0.10)** | 0.56 | 0.69 | 0.86 |
| Troubled vs. Complete Mental Health | ||||
| Intercept | 9.22 (0.81)** | |||
| Sprightliness | -3.49 (0.25)** | 0.01 | 0.03 | 0.04 |
| Integrity | 0.99 (0.22)** | 1.73 | 2.69 | 4.19 |
| Serenity | -0.61 (0.16)** | 0.39 | 0.54 | 0.74 |
| Moderation | -0.11 (0.15) | 0.65 | 0.89 | 1.22 |
| Humanity | 0.08 (0.17) | 0.77 | 1.08 | 1.52 |
Note. CI = confidence interval; LL = lower limit of CI; UL = upper limit of CI.
*p < .05. **p < .01.
Discussion [TOP]
The main objective of this research was to study the role that PPM traits play in the state of complete mental health. To begin with, the link between positive personality traits and mental health was explored by analysing their associations with a general measure of symptoms and one of well-being. As expected, positive correlations with the well-being measure and negative correlations with the psychopathological variable were observed. In agreement with a previous study on the PPM model (de la Iglesia & Castro Solano, 2018), positive traits were found to predict the presence of mental health. No other previous research that specifically used PPM may be used to compare these results since PPM postulation is relatively new. However, given the notion of a continuum with FFM, some results may be extrapolated and compared. Neuroticism is known to positively correlate with psychological symptoms, while consciousness, agreeableness and extraversion are known to negatively correlate with psychological symptoms (e.g. Habibi, Sadeghi, Haghrangbar, Madanipour, & Azarnoosh, 2013; Kotov, Gamez, Schmidt, & Watson, 2010; Malouff, Thorsteinsson, & Schutte, 2005). The opposite pattern has been found to occur between FFM traits and well-being (Joshanloo & Nosratabadi, 2009; Lamers, 2012; Lamers, Westerhof, Kovács, & Bohlmeijer, 2012). Therefore, the association pattern of PPM traits with psychological symptoms and well-being does not come as a surprise since it intrinsically shows that the presence of these traits is accompanied by the presence of well-being and the absence of psychological symptoms. Therefore, PPM traits probably function as protective factors of mental health.
However, this research emphasised the importance of studying mental health from a model that assesses both psychopathological symptoms and well-being signs conjointly. To do this, different clusters of mental health were obtained by combining the symptoms with the well-being measure. The four isolated groups replicated those proposed by the DFM (Greenspoon & Saklofske, 2001): complete mental health, symptomatic but content, vulnerable and troubled. In other words, the same configuration that was found in many other research studies (e.g. Eklund et al., 2010; Lyons et al., 2012; Suldo & Shaffer, 2008) was replicated here, thus giving the DFM more empirical evidence.
Then, the results of the MANOVAs showed that the groups differed in the presence of positive traits. As expected, the complete mental health group had a greater presence of sprightliness, integrity, serenity and moderation than the other groups. This is in agreement with previous studies, where the complete mental health group showed better results in different outcome variables (Antaramian, 2015; Antaramian et al., 2010; Eklund et al., 2010; Guerra Vargas, 2017; Keyes, 2004; Lyons et al., 2012; Smith, 2018; Suldo & Shaffer, 2008; Suldo et al., 2011). It also supports the main hypothesis of the PPM that the presence of these positive traits is associated with higher mental health, and therefore, the model can be used as a sanity nosology.
Finally, the multinomial logistic regression indicated that the PPM traits sprightliness and serenity increased the odds of belonging to the complete mental health group while humanity and integrity decreased these odds. This goes in line with the findings regarding FFM (Lyons, Huebner, Hills, & Shinkareva, 2012; MacMahan, 2013), where neuroticism (serenity in PPM) decreased the odds of belonging to the complete mental health group, but it contradicts the precedent of extraversion (humanity in PPM) increasing these odds. On the one hand, sprightliness and serenity continue to prevail as the most important traits of PPM in terms of mental health. On the other hand, integrity–a trait involving honest, sincere, reliable and humble behaviour–and humanity–a trait involving sensitivity to the individual´s context, a tendency to detect others’ needs and act in order to help them–were less likely to belong to the complete mental health group. This finding raises the question of the cultural aspects that may moderate the relation of these traits to positive outcomes. Does this phenomenon occur only in Argentina? In their pursuit of a better life in Argentina, do individuals commit dishonest and selfish acts? Are dishonesty and selfishness rewarded in in this country? Or are honest and altruistic acts not rewarded at all or not rewarded enough? This research suggests that Argentineans who act with integrity and humanity are less likely to have complete mental health. Future research should investigate whether this pattern replicates in other cultures.
This research does not go without limitations. The conceptualisation of traits may suggest some sort of casual thinking between the variables studied, but the cross-sectional design of the research prevents us from engaging in any possible causal interpretations. In addition, the sample mostly represents educated and middle-SES subjects and this hampers the generalisation of the study. Finally, the novelty of both PPM and DFM proposals is reflected in the few precedents in the literature and the abundant parallelism with similar or disaggregated models.
To conclude, this research gives further support to two important ideas. First, the study of mental health should include both psychopathological symptoms and well-being signs. The results obtained by the initial bivariate correlations are similar but not equal to the results obtained in the conjoint analyses. Second, positive traits continue to show an important role in different life outcomes. Personality assessment should most definitely include a sanity nosology.

 Contents
Contents This is an open access article distributed under the terms of the Creative Commons
Attribution License (
This is an open access article distributed under the terms of the Creative Commons
Attribution License (